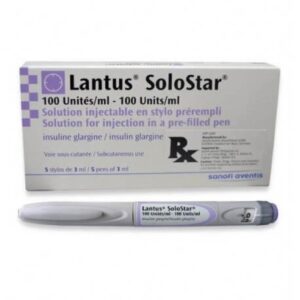
Lantus Cartridges (100 Units/mL)
$179.00
Please Note:
As part of our commitment to safe and responsible use, you must be 19 years of age or older to enter this site. It is illegal for a person under 19 years of age to purchase or attempt to purchase anything from insulining.com; and it is illegal to purchase for minors. All sales are conditional on the purchaser and recipient being of legal age. For information about age restriction, please contact Us
Lantus Cartridges (100 Units/mL) are only suitable for injecting just under the skin using a reusable pen. Speak to your doctor if you need to inject your insulin by another method.
Insulin glargine controls high blood glucose levels for adults and children over the age of 6 with type 1 and type 2 diabetes.
This medication is long-acting insulin that is similar to the insulin produced by the pancreas in our body. It begins working several hours after injection and continues to work evenly for 24 hours.
Lantus cartridges are made specifically to connect with certain insulin pens (including Lantus Solostar Pens)
This insulin may be recommended to be combined with oral diabetes medication or fast-acting insulin.
Taking insulin should only be part of your treatment. Patients should also incorporate a lifestyle that includes a healthy diet and regular exercise. Lantus Cartridges (100 Units/mL)
Each ml contains 100 units insulin glargine* (equivalent to 3.64 mg).
Each cartridge contains 3 ml of solution for injection, equivalent to 300 units.
*Insulin glargine is produced by recombinant DNA technology in Escherichia coli.
For the full list of excipients, see section 6.1.
Solution for injection.
Clear colourless solution.
Treatment of diabetes mellitus in adults, adolescents and children aged 2 years and above
Hypersensitivity to the active substance or to any of the excipients listed in section 6.1.
In order to improve the traceability of biological medicinal products, the name and the batch number of the administered product should be clearly recorded.
Lantus is not the insulin of choice for the treatment of diabetic ketoacidosis. Instead, regular insulin administered intravenously is recommended in such cases.
In case of insufficient glucose control or a tendency to hyper- or hypoglycaemic episodes, the patient’s adherence to the prescribed treatment regimen, injection sites and proper injection technique and all other relevant factors must be reviewed before dose adjustment is considered.
Transferring a patient to another type or brand of insulin should be done under strict medical supervision. Changes in strength, brand (manufacturer), type (regular, NPH, lente, long-acting, etc.), origin (animal, human, human insulin analogue) and/or method of manufacture may result in the need for a change in dose.
Patients must be instructed to perform continuous rotation of the injection site to reduce the risk of developing lipodystrophy and cutaneous amyloidosis. There is a potential risk of delayed insulin absorption and worsened glycaemic control following insulin injections at sites with these reactions. A sudden change in the injection site to an unaffected area has been reported to result in hypoglycaemia. Blood glucose monitoring is recommended after the change in the injection site, and dose adjustment of antidiabetic medications may be considered.
Hypoglycaemia
The time of occurrence of hypoglycaemia depends on the action profile of the insulins used and may, therefore, change when the treatment regimen is changed. Due to more sustained basal insulin supply with Lantus, less nocturnal but more early morning hypoglycaemia can be expected.
Particular caution should be exercised, and intensified blood glucose monitoring is advisable in patients in whom hypoglycaemic episodes might be of particular clinical relevance, such as in patients with significant stenoses of the coronary arteries or of the blood vessels supplying the brain (risk of cardiac or cerebral complications of hypoglycaemia) as well as in patients with proliferative retinopathy, particularly if not treated with photocoagulation (risk of transient amaurosis following hypoglycaemia).
Patients should be aware of circumstances where warning symptoms of hypoglycaemia are diminished. The warning symptoms of hypoglycaemia may be changed, be less pronounced or be absent in certain risk groups. These include patients:
– in whom glycaemic control is markedly improved,
– in whom hypoglycaemia develops gradually,
– who are elderly,
– after transfer from animal insulin to human insulin,
– in whom an autonomic neuropathy is present,
– with a long history of diabetes,
– suffering from a psychiatric illness,
– receiving concurrent treatment with certain other medicinal products (see section 4.5).
Such situations may result in severe hypoglycaemia (and possibly loss of consciousness) prior to the patient’s awareness of hypoglycaemia.
The prolonged effect of subcutaneous insulin glargine may delay recovery from hypoglycaemia.
Related products
Insulin
Insulin
Insulin
Insulin
Insulin
Diabetes Supplies
Insulin
Diabetes Supplies
Insulin
Diabetes Supplies
Insulin
Insulin